 21 September 2022
21 September 2022
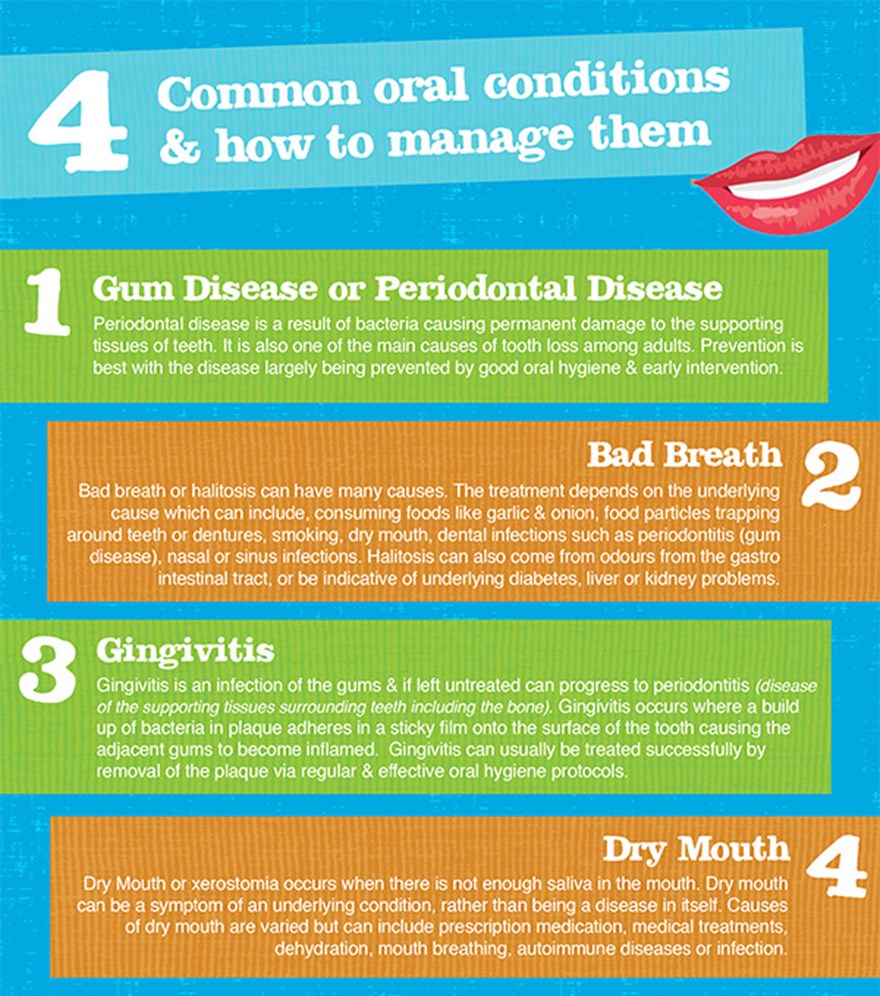
Do you have oral symptoms and aren’t sure if they are normal? Could they be the sign of some other underlying condition? Read about 4 common oral conditions, symptoms you shouldn’t ignore and how to help keep your teeth and gums healthy.
Dry Mouth
Dry Mouth or xerostomia occurs when there is not enough saliva in the mouth. Dry mouth can be a symptom of an underlying condition, rather than being a disease in itself. Causes of dry mouth are varied but can include prescription medication, medical treatments, dehydration, mouth breathing, autoimmune diseases or infection.
Common Signs and Symptoms of Dry Mouth include:
- A sticky or dry feeling in the mouth or throat
- Frequent thirst
- Split skin at the corners of the mouth or cracked lips
- A burning or tingling sensation in the mouth or the tongue
- A rough, dry, red, or raw tongue
- Mouth ulcers
- Bad breath
- Oral Thrush or infections of the Salivary Glands
- Difficulty with speech, taste, chewing or swallowing
- Difficulty wearing dentures
Xerostomia can also lead to an increase in cavities, as saliva also plays a role in protecting teeth against caries.
Treating options for dry mouth depend upon the underlying cause and may include options such as changing medication or dosages, treating any infections present and attempting to increase saliva production.
Where the xerostomia is a result of an underlying condition and not necessarily able to be reversed/treated definitively, the symptoms can be treated to provide relief. Options for managing symptoms include sipping water regularly, use of non alcoholic mouthwash and gels containing a lubricant and use of commercially available salivary substitutes.
Patients with xerostomia should also avoid caffeine, alcohol, smoking, dry or spicy foods.
If you’re experiencing dry mouth it is best to book a dental appointment to investigate any potential causes and discuss solutions.
Bad Breath
Bad breath or halitosis can have many causes. The treatment depends on the underlying cause which can include, consuming foods such as garlic and onion, food particles trapping around teeth or dentures, smoking, dry mouth, dental infections such as periodontitis (gum disease), nasal or sinus infections. Halitosis can also come from odours from the gastro intestinal tract, or be indicative of underlying diabetes, liver or kidney problems.
Halitosis is most commonly caused however by sulphur-producing bacteria that normally live on the surface of the tongue and throat. According to Better Health Victoria, about 2.4% of the population suffers from halitosis.
Halitosis Symptoms can include:
- A dry mouth
- A white coating on the tongue
- Build up of plaque and calculus or food debris around teeth
- A burning tongue
- Thick saliva
- A constant need to clear your throat
- A constant sour, bitter metallic taste
Treating halitosis depends on the underlying cause but good oral hygiene, including tongue brushing is an important first step. The use of tongue scrapers as well as mouthwashes, lozenges and toothpastes can help remove bad breath. Drinking water frequently can also assist by removing any stagnated saliva which can contribute to bad breath and is one of the common causes for “morning breath”.
It is important to consult your dentist to find the most effective treatment for you.
Gingivitis
Gingivitis is an infection of the gums and if left untreated can progress to periodontitis (disease of the supporting tissues surrounding teeth including the bone). Not all gingivitis progresses to periodontitis and by itself is usually reversible. Gingivitis occurs where a build up of bacteria in plaque adheres in a sticky film onto the surface of the tooth causing the adjacent gums to become inflamed. Gingivitis can usually be treated successfully by removal of the plaque via regular and effective oral hygiene protocols.
Gingivitis Symptoms may include:
- Gums that bleed when brushing or flossing
- Gums that are red, tender or swollen
- Gums that have pulled away from the teeth
- The presence of pus or exudate between teeth and gums
- Pain when chewing
- Sensitive or loose teeth
If gingivitis is left untreated it can advance to Periodontal Disease (often referred to as gum disease).
There are a variety of treatment options for Gingivitis, which usually involve removal of any plaque build ups and of any rough edges of fillings which provide a safe haven for the build up of plaque. If you have any gingivitis symptoms make sure you get a dental check-up.
Gum Disease or Periodontal Disease
According to the World Health Organisation 15-20% of middle aged (35-44 year olds) adults have severe periodontal disease. Periodontal disease is a result of bacteria causing permanent damage to the supporting tissues of teeth. Periodontal disease is also one of the main causes of tooth loss among adults. Prevention is best with the disease largely being prevented by good oral hygiene and early intervention when problems are identified.
Some people are more at risk of gum disease for example: people with poor oral hygiene or a disability making teeth cleaning difficult, people who smoke, people with diabetes and females during pregnancy.
According to the Australian Dental Association the following are possible symptoms of periodontal disease:
- Bleeding gums when you brush your teeth
- Bad breath or a bad taste in your mouth
- Receding gums
- Sensitive teeth or gums
- Loose teeth or teeth that have moved
Gum Disease Treatment: General dentists are trained in managing periodontal problems, however you may be referred to a Periodontist if your condition needs more advanced care. If you have any dental concerns or are due for a dental check up book a dental appointment at your local dental centre.





